Leisure should lead in treating and preventing obesity
Obesity is a major public health concern in the UK and a government health policy priority (UK Government, 2020). Increasing rates of obesity in the UK are storing up problems for individuals and the health service. It is estimated that overweight and obesity related conditions across the UK are costing the NHS £6.1 billion each year.
In fact, obesity is associated with reduced life expectancy and is a risk factor for chronic disease including cardiovascular disease, type 2 diabetes, cancer, liver and respiratory disease, and can also impact on mental health.
According to NHS England one in four adults in the UK is obese, up from 13% of men and 16% of women in 1993 (NHS England, 2019). This impacts on many areas of life and the economy, including increased demand on the NHS.
The latest NHS Digital report “Statistics on Obesity, Physical Activity and Diet, England 2021”, shows 1.02 million hospital admissions where obesity was a factor for the year 2019 to 2020. This is an increase of 17% from 2018/19 and is in addition to the 10,780 admissions directly attributable to obesity. Around two thirds (64%) of admissions where obesity was a factor were female. (NHS Digital, 2021).
Age as a factor in obesity related hospital admissions
Sixty nine percent of admissions directly attributable to obesity (such as for bariatric surgery) were in the age range 35 to 64, with a peak (3,107) for patients aged 45 to 54.
Where obesity was a factor in the cause for admission, rather than the direct cause, the age distribution could be viewed in two ways: either as a more uniform distribution; or as a peak at 65 to 74 with a spike in the trend for those aged 25 to 34.

Acknowledgement: (NHS Digital, 2021)
In either case preventative exercise could relieve pressure on NHS services, particularly in the 55+ age group where a relative weighting in admissions is observed: of the 1.02m admissions where obesity was a factor, 516,795 (50.6%) were aged over 55 years.
The lower incidence in the 35 to 54 age groups may be attributable to active work and lifestyles, whilst the high number of admissions for people aged 25 to 34 is interesting: data within the report shows high numbers of obesity related complications during pregnancy or maternity. Whether this is significant could be analysed further.
As the front line of the NHS (our recent blog), the leisure sector should be viewed as an asset that provides sustainable, preventative exercise solutions for everyone living with obesity. Considering the age profile of admissions where obesity is a factor, there also needs to be a greater emphasis on accessible exercise for older adults, a market which also provides new commercial benefits for leisure operators yet is consistently overlooked as we have discussed in previous blogs (Shapemaster Global, 2020).
Taking up exercise even in later life provides strong benefits in terms of reversing or slowing down the onset or progression of various health conditions and reducing the impact of the normal ageing process. (Taylor, 2014)
Deprivation
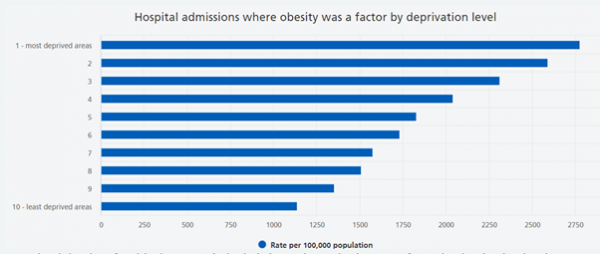
There is a clear link between social inequality and hospitalisation caused by obesity. Admissions where obesity was a factor were over twice as likely in the most deprived areas (2,778 per 100,000 population), compared to the least deprived areas (1,139 per 100,000 population).
Part of the government’s ‘levelling up’ agenda seeks to address this and there are excellent examples of public sector leisure operators and local authorities who are increasing access to exercise as solutions for the problems linked to deprivation.
Older adults in deprived areas need greater opportunities to benefit from the health, social and wellbeing benefits that exercise and active ageing can provide.
Effect of obesity on Covid-19 outcomes
Various studies have shown a greater tendency for obese people to become severely ill with Covid-19, require hospitalisation or have an increased risk of death, compared with those not classed as obese (Sameer Mohammad, 2021). Inactive people also carry greater risks of severe Covid-19 outcomes. In one study, 84 out of 124 patients requiring mechanical ventilation had a Body Mass Index of over 30kg/m2. Obesity is known to increase vulnerability to other conditions and reduced immune response, which in turn increases the risk of serious outcomes for Covid-19.
It is therefore crucial at this time that exercise should be more widely encouraged, as part of an overall approach to reduce and manage obesity.
Long Covid
In a study of 2,839 people who tested positive for Covid-19, 44% required hospital admission 10 months after testing positive, showing signs of long-term complications or Long-Covid. Whilst this percentage is worryingly high, mildly obese patients were 28% more likely to develop such Long-Covid symptoms, whilst those with severe obesity were 30% more likely to develop long-term complications and sustained illness (Cleveland Clinic, 2021).
Vaccine effectiveness
A study, which is yet to be peer reviewed, indicates that the Pfizer/BioNTech vaccine may be less effective in people classed as obese, with only half the antibodies produced compared with healthy people (Pellini, 2021). Excess body fat can cause metabolic changes such as insulin resistance and inflammation, which make it more difficult for the body to fight infection.
Ongoing low-level inflammation can weaken certain immune responses, including those launched by the B and T cells that trigger a protective response following vaccination. Separate research shows that the flu vaccine is only half as effective in obese people compared to those of healthy weight.
Exercise: a miracle cure at the front line of the NHS
We continue our call on the government to embed the role of physical activity in a policy statement to which ministers should adhere when developing proposals in the policy paper: “Transforming the public health system: reforming the public health system for the challenges of our times”.
The disruption caused by the global pandemic has taught us to be innovative and shake up the status quo. With a greater emphasis on preventative exercise, the nation can be more resilient to future waves of illness such as Winter Flu and Covid-19; but we must also wake up to those silent killers like obesity, caused partly by inactivity and poor recognition of the miracle cure available to all of us to some degree.
With two thirds of adults and a third of children classed as overweight – and therefore potentially on a path to obesity – there is latent demand on the NHS building up that needs preventative, age-appropriate and whole system action now, with leisure at the heart of it… and at the front line.
- 67yrs Average age of Shapemaster users across the UK
- 70% of customers say they can now move around better
- 75% Say they visit a Shapemaster Studio 3 times a week.
- 90% of Shapemaster users say it improves their mental health
Sources:
NHS Digital. (2021). Statistics on Obesity, Physical Activity and Diet, England 2021
Pellini, R. (2021). Obesity May Hamper SARS-CoV-2 vaccine immunogenicity.
Shapemaster Global (2020). Shapemaster is the Right Investment at the Right Time
Shapemaster Global (2021). Leisure – The Front Line of the NHS