Leisure – the frontline of the NHS
At the 2016 ukactive National Summit, NHS England Chief Executive Sir Simon Stevens addressed leisure sector leaders at the Queen Elizabeth II Centre to emphasise the importance of leisure in protecting the NHS.
His plea: “We need you” to help reduce and prevent illness and injury and relieve pressure on the National Health Service.
Just over three years later, the world would be on the brink of a global pandemic and his words would have more importance than one could have imagined at the time.
Having led NHS England since 2014 and guided the service through the pandemic and the hugely successful vaccine rollout, Sir Simon will step down as Chief Executive in July 2021.
Sir Simon’s legacy includes his call for more joined-up working between councils running social care and their local NHS counterparts, which resulted in the creation of ‘integrated care systems’ in England. As an industry, we must now add to this legacy the realisation of physical activity as the vital front line of the NHS.
We, along with many industry colleagues, call on the government to embed the role of physical activity in a policy statement that ministers must adhere to when developing proposals outlined in the policy paper: “Transforming the public health system: reforming the public health system for the challenges of our times”.
Encouraging active ageing is especially important as people are living longer, thereby naturally placing a greater demand on NHS services. We outline some examples from a growing body of evidence of the importance of exercise in preventing or managing illness, injury or long-term conditions.
The current health crisis
A study published in the British Journal of Sports Medicine, April 2021, identified that people who were consistently meeting recommended physical activity guidelines were less likely to be hospitalised, admitted to intensive care (ICU) or die from COVID-19 related illness than those who were consistently inactive or doing some activity. A similar trend was observed for those who were doing some activity compared with those who were consistently inactive.
Hospitalisation
People who are consistently inactive are 2.26 times more likely to be admitted to hospital compared with those consistently meeting physical activity guidelines.
Intensive care unit admission
People who are consistently inactive are 1.73 are times more likely to be admitted to ICU compared with those consistently meeting recommended activity guidelines.
Covid-related death
People who are consistently inactive have 2.49 greater odds of death compared with patients who were consistently meeting activity guidelines.
The wider health picture…savings to the NHS from prevention
In its 2018 Reimaging Ageing report, ukactive collaborated with Sheffield Hallam University and Datahub to estimate potential cost savings with a comprehensive transformation of the activity sector and a greater proportion of older people supported to be more physically active.
The headline result is that £7.67 billion over 10 years could be achieved in NHS and healthcare savings if one third of inactive over 55s were supported into sustainable physical activity.
This would result from a reduction in the cost of treatment from lower incidence of six physical inactivity related long-term conditions, and the associated reduction in GP visits.
As Prof Chris Whitty stated at the 2020 virtual ukactive National Summit, “There is no point in life where doing more exercise does not improve health in multiple ways.”
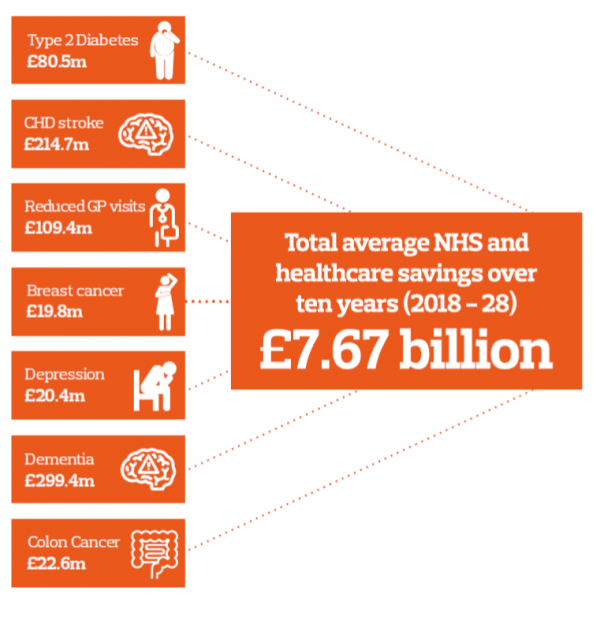
Acknowledgement: Reimaging Ageing, ukactive 2018
Recent Studies
Heart patients advised to move more to avoid heart attacks and strokes
Research presented at the online 2021 preventative cardiology meeting of the European Society of Cardiology demonstrated that increased activity can reduce risk of heart disease and mortality for people living with elevated blood pressure, high cholesterol and diabetes.
Of the 88,320 subjects, 18,502 (21%) had high blood pressure, high cholesterol, and/or diabetes at the start of the study. The average age of this group was 55. Adjusting for age, sex, and baseline physical activity, the evidence indicated that participants who experienced moderate to large improvement in physical activity were around 30% less likely to develop cardiovascular disease or die during follow-up compared to those who did not improve their activity level.
The study’s author Dr Esmée Bakker highlighted the importance for inactive people to begin with a gentle, entry level exercise, while those who are fairly active should try doing 10 minutes more each day or increasing the intensity.
“As people get older and their bodies decline in function, physical activity helps to slow that decline… It’s important they remain active or even increase their activity as they get older.” Dr Nick Cavill, health-promotion consultant.
Exercise and cancer
Over the last three years, GM Active, the collective of leisure operators in Greater Manchester, has been supporting Manchester residents with a new cancer diagnosis, to better prepare for surgery and subsequent treatment through their highly commended Prehab4Cancer programme. Delivering a combination of specialist exercise advice and classes, nutritional information and psychological support, Prehab4Cancer aims to improve post-surgery recovery times and overall outcomes for its participants.
This approach has subsequently been taken up by the Advanced Wellbeing Research Centre at Sheffield Hallam University in a pilot due to begin in autumn.
Professor Robert Copeland, Director of the Advanced Wellbeing Research Centre, said: “We want to help improve the way we support people with cancer to prepare for and recover from their treatment.
“Being more physically active following a cancer diagnosis is associated with a lower risk of cancer recurrence and a greater likelihood of recovery.
“Physical activity is not usually prescribed for patients receiving cancer treatment and we want that to change.”
Physical activity must be at the front line in delivering current and future health agendas. As a sector we need to work collectively to ensure it achieves the political and public voice required to make it happen.
‘Improving health – and active ageing – needs to be viewed as an investment, and not as a cost!’.
- 67yrs Average age of Shapemaster users across the UK
- 70% of customers say they can now move around better
- 75% Say they visit a Shapemaster Studio 3 times a week.
- 90% of Shapemaster users say it improves their mental health